Juvenile Macular Degeneration: Symptoms, Causes, Management, and More
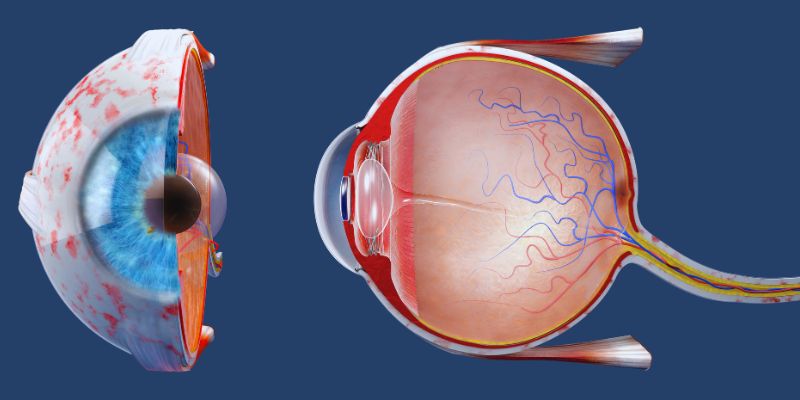
A group of eye diseases called juvenile macular degeneration (JMD) is passed down from parent to child and mostly affects kids and young people. These disorders damage the macula, a retina component in charge of sharp central vision, causing progressive vision loss.
JMD begins early in life and can greatly affect daily activities, including reading, driving, and face recognition, unlike age-related macular degeneration (AMD), which affects older persons. Early diagnosis and action depend on a knowledge of the symptoms, causes, and management techniques. Early discovery can help people impacted by development delays and enhance their quality of life.

Symptoms of Juvenile Macular Degeneration
The type of JMD and its degree determine how young macular degeneration presents symptoms. However, children and young adults who could have this disorder should be especially alert for some typical symptoms. Though they usually show slowly, these symptoms can greatly affect daily living once they start.
- Blurred Or Distorted Vision: JMD first appears to have trouble seeing clearly. Straight lines may seem twisted, and objects may seem wavy or hazy.
- Difficulty Focusing Or Reading: As the macula, which regulates acute center vision, becomes compromised, people with JMD often find it difficult to read or focus on minute details.
- Loss Of Central Vision: JMD can cause a slow loss of central vision over time, which is required for jobs including reading and face recognition. Usually, peripheral vision stays unchanged.
- Light Sensitivity: Those with juvenile macular degeneration may be more sensitive to light, particularly in strong illumination or sunlight.
- Color Vision Changes: Some people's color vision changes, making it more difficult to tell one hue from another.
These signs range from moderate to severe and could develop gradually. Early identification is crucial for good care and the preservation of as much eyesight as possible.
Causes of Juvenile Macular Degeneration:
Each of the many forms of JMD is connected to particular genetic alterations. Though they all impact the macula differently, the most common JMD are Stargardt disease, Best disease, and juvenile retinoschisis, which cause similar vision impairments.
- Stargardt Disease: Mutations in the ABCA4 gene produce this most common JMD. A protein produced by the ABCA4 gene helps the retina eliminate waste materials. Waste materials gather and compromise the macula when this gene mutates.
- Best Disease: Mutations in the BEST1 gene define Best disease, sometimes called Best vitelliform macular dystrophy. Under the retina, this disorder causes a yellowish cystlike lesion to develop, progressively compromising vision.
- Juvenile Retinoschisis: Mutations in the RS1 gene produce this disorder, which alters the retina's capacity to send signals to the brain. It causes the layers of the retina to split, increasing visual loss.

Management of Juvenile Macular Degeneration:
Though there is no treatment for young macular degeneration, several approaches can help control the disorder and extend eyesight for as long as feasible. Implementing a good management strategy that can slow down disease development depends on early diagnosis.
- Low Vision Aids: Devices such as magnifying glasses, specialized reading software, and improved lighting can help those with JMD maintain independence and more easily complete daily tasks.
- Vision Rehabilitation entails working with a specialist who can teach people how to adjust to vision loss by learning new strategies for reading, writing, navigating their surroundings, and using their residual sight more effectively.
- Regular Eye Exams: Regular eye exams let early vision changes be found and allow treatment plan adjustments as necessary. Keeping an eye on the disease's development will enable one to customize the treatment for every person's needs.
- Genetic Counseling: Genetic counseling can provide families with a history of JMD with important information about their chances of passing the disorder to the next generation. It also provides direction on early diagnosis and treatment.
- Emerging Treatments: Research is underway to identify fresh approaches for young macular degeneration. Certain experimental treatments, including stem cell and gene therapies, show promise in stopping or slowing down the course of the illness. However, these medicines are still in the early phases of research.
Differences between juvenile and age-related AMD:
While age-related macular degeneration and juvenile macular degeneration compromise the macula and cause central vision loss, there are significant distinctions between the two diseases.
- Age Of onset: While AMD usually affects older persons, commencing about age 50 or older, juvenile macular degeneration frequently starts in childhood or early adulthood.
- Genetic Component: While AMD is impacted by a mix of genetic and environmental elements, including smoking, food, and sun exposure, JMD is brought on by inherited genetic abnormalities passed down through families.
- Progression Rate: Though this varies based on the type of JMD and the person, JMD usually advances more slowly than AMD. While some types of JMD may advance more slowly, others can cause fast vision loss.
- Treatment Options: Although antiVEGF injections and other drugs slow the course of AMD, there are not yet FDA-approved therapies for JMD. Still, low vision aids and rehabilitation can help control symptoms of both diseases.
Living with Juvenile Macular Degeneration:
For children, young people, and their families, living with juvenile macular degeneration offers special difficulties. Gradual loss of eyesight can compromise schooling, employment, and social events, impairing people's ability to lead autonomous lives. Many persons with JMD, however, may keep a satisfying lifestyle with the correct tools and assistance.
- Support Groups: For those with JMD and their families, attending a support group offers emotional and pragmatic help. It might be rather helpful to share difficulties with someone going through similar ones.
- Educational Accommodations: Schools and colleges sometimes provide accommodations such as larger text materials, audiobooks, and more time on tests to help kids with JMD achieve academically.
- Workplace Adaptations: Assistive technologies, flexible working schedules, and modified desks to meet visual demands could help JMD employees in the workplace.
Those with JMD can keep leading active and satisfying lives by being educated and using the resources.
Conclusion:
The difficult disorder, juvenile macular degeneration, strikes young people and causes increasing visual loss. Early diagnosis and suitable treatment plans can assist in maintaining vision and enhance quality of life even if there is no cure. Those with JMD can continue flourishing despite obstacles with the correct tools, help, and new treatments. Managing young macular degeneration requires a proactive strategy to adjust to vision loss and keep current with future developments.